 |

|
 |

|
 Back to 2000 4th Quarter Table of Contents
Back to 2000 4th Quarter Table of Contents
Introduction I became interested in vitamin C in 1951 because as an antioxidant it inhibits the oxidation of adrenalin to adrenochrome. I used doses of three grams per day and more for my schizophrenic patients. In 1952, I gave one gram each hour for 48 hours to a woman who had become psychotic after a mastectomy and had been admitted on a Thursday for electro-convulsive treatment, the only treatment then which had any effectiveness. Monday morning after that vitamin C weekend she was mentally normal and did not need the ECT. At the same time her ulcerated, infected mastectomy lesion had begun to heal. She died six months later from her cancer but mentally normal. This showed that huge doses of vitamin C were tolerable and potentially valuable in treating psychotic patients. In 1960, a 75-year-old psychotic retired professor was admitted to our psychiatric ward. He had terminal, inoperable lung cancer identified by x-ray and biopsy but he also excreted large amounts of a substance in his urine we had found present in most of our schizophrenic patients. These patients responded well to treatment with vitamin B3. I therefore started him on niacin (B3) 1 g three times daily and the same amount of vitamin C. A few days later he was mentally normal. Every three months his lesion was smaller on x-ray examination and after one year was gone. He died 30 months after I first saw him. A year or two later a 16-year-old female with Ewing’s sarcoma was slated for surgery to amputate her arm. I started her on niacinamide 1g three times daily and ascorbic acid 1 g three times daily and suggested to the surgeon he postpone surgery. Her cancer disappeared. In 1977, a female with jaundice was found to have a large mass in the head of the pancreas. It was inoperable, was not biopsied because of the danger of spreading the disease and she was advised she might survive six months. She 1. #3A-2727 Quadra St., Victoria, BC V8T 4E5 began to take 10 grams of vitamin C each day and later was referred to me. I increased it to 40 grams and added several other vitamins. She is alive today. What are the odds that the first four terminal cases of cancer I saw would all respond to simple vitamin therapy? If the woman last referred to had died, as it was expected she would, I would not be at this Vitamin C and Cancer Workshop, for she told so many people about her recovery that within a few years many patients were routinely referred to me. I am a psychiatrist who was involved with Linus Pauling in establishing orthomolecular psychiatry and medicine. I had been routinely using several nutrients in my treatment protocols which included vitamin B3 (niacin or niacinamide), vitamin C, pyridoxine, B complex preparations, vitamin E, and zinc. Patients were all referred by their family physicians or surgeons as is the custom for all British Columbia specialists. Before patients could see me they had to be referred by their general practitioner. This was very difficult for most of the patients since their primary problem was not psychiatric even though they all suffered from various degrees of anxiety or depression, not surprising when confronted with a terminal disease. Only the dedicated patients broke through that barrier. Over half the patients told me when they arrived how much difficulty they had had in obtaining the referral. Over the past five years it has been much easier for them as the degree of acceptance increased in Victoria, where I practise. Another fact was that very few of the physicians had heard anything about the use of megadose vitamins, especially for the treatment of cancer and they were very skeptical. I know that many patients did not have the strength or tenacity nor enough support from their families to run the gauntlet and therefore did not ever get referred to me. In my opinion only the very highly motivated patients made the effort and I believe their motivation was stimulated by the prognosis given them, usually dismal, and by the severity of their disease. Patients given a good prognosis and responding well to standard treatment would have no reason to see me. My interest in using nutrients was well known and this made it somewhat simpler for these physicians to refer patients where psychiatric problems were minor compared to their physical concerns. I must add that I was not involved in investigating, diagnosing, nor in planning the orthodox treatment. This was done by the referring physicians and the local cancer clinic. Almost every patient received a combination of surgery, radiation and chemotherapy (Table 1, below). My experience with a few patients who had responded so well preconditioned me to look upon the Cameron/ Pauling studies very seriously. I advised all my cancer patients to improve the quality of their diet and to take 12 grams of vitamin C daily and to increase it to sublaxative levels whenever possible. I also added vitamin B3, beta carotene, and zinc. After I had seen about 50 patients I did a follow up on each of them. I found to my surprise and pleasure that the patients who had stuck with the program at least two months lived much longer than the smaller group who had not followed the program.1 This was not a randomized study and I had not planned it to be. It was the use of orthomolecular treatment for a group of desperate patients, most of them with terminal and untreatable forms of cancer. I am familiar with the double-blind methodology since under my direction in Saskatchewan we conducted the first six prospective, randomized, double-blind, therapeutic trials in psychiatry beginning in 1952, but in private practice I was not able to conduct this type of study.
Antioxidant Nutrients and Cancer By the end of 1998 I had treated over 1,000 cancer patients. Arising from this large cohort, I published various reports outlining my conclusions.2-8 The Control Group I hoped that every patient seen would follow the regimen but in fact they did not and it would have been very surprising if they had. Clinical research is messy. It is not the clean cut affair many theorists would have us think it is. I decided originally to use as my control every patient who did not follow the regimen for at least two months, including many who died within two months after they first saw me. They were still on standard treatment or had already received it and I considered that this group would constitute my control. I played no role in determining who would not follow the program. The decisions were made by fate, by referring physicians, by oncologists and by family members or by the belief the cost involved in taking nutrients was not justified. For this workshop I have excluded every patient who died within two months after first seeing me. This removes the argument that I had thrown the most hopeless group into the control group. Every patient who followed this program for at least two months was included in the treatment group and every patient who did not is included in the control group. It is not a randomized control group, nor would this have been possible in this series. I think it is fair to split the groups this way because, based on my experience, it takes about two months for the program to begin to take effect. Clinical Matters Fewer than 10 percent of the patients were early onset cases. The rest were all late stage, or inoperable, or untreatable, or had failed to yield to treatment, or had relapsed after having had treatment. The early cases were not motivated to come to see me and physicians did not tell the patients that vitamin treatment was an option. The desperate nature of the disease forced them all to consult with me when they had lost all hope of receiving any additional help. I used only hard data. This was the length of time these patients lived after they had first seen me. I did not and could not use size of tumor and other clinical criteria used by oncologists for evaluating the treatment. During the first interview I told the patients that I was not treating the tumor, that this was the responsibility of their oncologists, that I was offering them a nutritional program which I hoped would increase the probability of their survival. I pointed out that this was not an alternative treatment, that it was complementary. I added that the use of nutrients was compatible with any other treatment including surgery, chemotherapy and radiation. For many years I had to counteract the advice given these patients by the nutritionists at the cancer clinic and by their oncologist who insisted on telling them that the vitamins would interfere with the therapy. This is based upon their theoretical view that the antioxidants would decrease the effectiveness of the treatment in killing tumor cells. This is contradicted by the literature. In fact, vitamins increase the effectiveness of the treatment and decrease the toxic effect on the patient.9 I would see the patient again in one or two months to deal with any problems unless they were depressed or very anxious in which case I would treat them as primary psychiatric patients. Each year after they were first seen I would obtain a report of whether they were alive and how they were doing. I would call either the patient, their family, their physicians or the cancer clinic and I would check the obituaries in the local paper. Since over 90% of my patients came from southern Vancouver Island, almost all deaths are reported in the local daily paper. Results A comparison between the patients who followed the program and those who did not is given in Table 2, and in Figure 1 (below). Out of the original 134 patients three were lost to follow up. Nine died within the first two months and are excluded. I examined further the first cohort of 134 patients as of December 1998. Thirty-three were still alive from the treated group, all having survived at least ten years. None survived from the control group. Half the six deaths in 1992 were caused by other physical disease, not directly from cancer.
Figure 1. Comparison of cancer patients treated with standard or orthomolecular treatment, first ten years of study. 100 90 80 70 60 50 40 30 20 10 0
1 3579 years Antioxidant Nutrients and Cancer In Table 1 (p.194) I have shown some of the treatment variables for ten-year survivors. Only one was treated by orthomolecular treatment alone. The remainder had the usual standard treatments as determined by their oncologists and the cancer clinic they attended. The proportion of all the patients receiving these therapies is the same as it is for this smaller group of survivors. The survival trends which appeared in the first Hoffer and Pauling paper2 and reappeared in our second3 and in my third presentation are reconfirmed in this report. A comparison between the patients seen until the end of 1993 who followed the program and those who did not is given in Table 3 and in Figure 2 (below). A comparison between the patients seen until the end of 1997 who followed the program and those who did not is given in Table 4 and in Figure 3 (p.198). Special Cases Case 1. 63-year-old woman with poorly differentiated squamous cell carcinoma of the lung In November, 1983, the patient presented with constitutional symptoms and collapse of the upper lobe of the right lung. Bronchos-copy and mediastinoscopy were negative, but at thoracotomy in December, 1983, she was found to have a poorly differentiated squamous cell carcinoma occluding the right upper lobe bronchus and extending to the lateral chest wall. She was deemed inoperable and was given a course of 20 sessions of cobalt irradiation to her right chest (January, February, 1984). In April, 1984 she began a vitamin regimen including vitamin C, 12 g, niacinamide 1.5 g, and other vitamins. Chest x-rays in 1984 and 1985 showed extensive pleural thickening at the right lung base and fibrotic scarring extending into the right apex. Table 3. All patients seen before the end of 1993 (excluded, 48).
Figure 2. Comparison of cancer patients treated with standard or orthomolecular treatment, seen before the end of 1993. 100 90 80 70 60 50 40 30 20 10 0 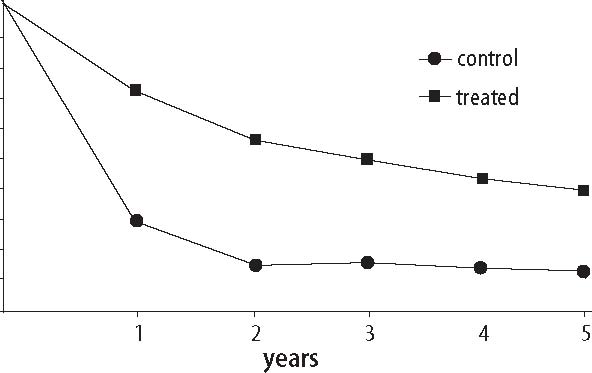 The patient continued to take 12 g of vitamin C per day until 1987, after which she reduced the dose to 8 g per day. She was discharged from the Victoria Cancer Clinic in 1988 as not requiring further follow up. She had a mild stroke in January, 1993, and a more severe one in December of that year. She died in January, 1994, without evidence of cancer 10 years after diagnosis. Case 22. 14-year-old girl with Ewing’s sarcoma of the left humerus This patient presented to hospital in October, 1979, with a painful left upper arm. There was obvious bony swelling of the upper half of the humerus. The x-ray was highly suggestive of Ewing’s sarcoma, a diagnosis confirmed on open biopsy. There was no evidence of tumor spread and she underwent radiotherapy and multiple courses of chemotherapy over a period of two years, including cyclophosphamide, vincristine, actinomycin D, and doxorubicin. During the period of therapy she developed a displaced fracture at the site of the sarcoma and in 1981 consideration was given to the possibility of residual tumor. She was started on 12 g of ascorbic acid, 3 g niacinamide, 250 mg pyridoxine, in July, 1981.In 1982 there was evidence of spontaneous healing at the fracture site and no evidence of recurrent malignant disease and she remains disease-free. She stayed on a megavitamin regimen from 1981-83, with her vitamin C intake ranging from 4-16 g/day. She may be considered cancer free after a 20 year period without disease. Case 23. 39-year-old woman with carcinoma of the ovary The patient presented to hospital in 1981 with ascites and a 10 X 12 cm pelvic tumor, found on operation to be a Stage IIC
Figure 3. Comparison of cancer patients treated with standard or orthomolecular treatment, seen before the end of 1997. 100 90 80 70 60 50 40 30 20 10 0 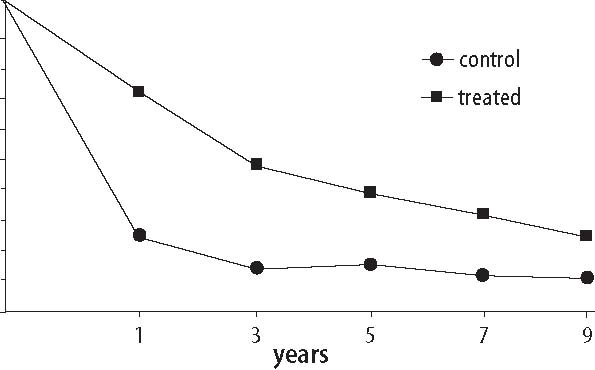 Antioxidant Nutrients and Cancer non-mucin secreting adenocarcinoma involving a fallopian tube. A hysterectomy and bilateral oophorectomy and omentectomy were carried out. Over the year 1981, she received chemotherapy with cisplatin and doxorubicin, followed by radiation therapy to the anterior abdomen and pelvis in October 1981 after which she was disease free. In May 1982 she was begun on a vitamin regimen that included 12 g vitamin C, 1.5 g niacinamide, 250 mg pyridoxine, 220 mg zinc sulfate, and vitamin A. She followed the program for about one year, after which she took the vitamins only intermittently. In 1995 she underwent a posterior craniotomy to remove a tumor in the left cerebellum. This was found to be a papillary adenocar-cinoma. The patient then received radio-therapy to the brain. She resumed vitamin therapy, and was well in 1998. Case 74. 35-year-old man with widespread multiply recurrent lymphoma. In 1983 this patient was found to have a poorly differentiated small cell small non-cleaved lymphoma involving his retro-peritoneum, diagnosed at laparotomy. A CT scan revealed a retro-pancreatic mass 12 cm in diameter extending into the mesentery. Over the next two years he received several courses of chemotherapy (including doxorubicin, cyclosphosphamide, vincristine, and prednisone) and several courses of radiotherapy for the original tumor and its multiple recurrences. In March, 1984, a recurrence in the left posterior chest wall was treated with radiotherapy. In May, 1984, a recurrence in the left thoracic spine was treated with radiotherapy and chemotherapy. A large right pelvic mass detected in January, 1985, was treated with radiotherapy. Progress notes in the medical record between 1983-84 consistently note his dismal prognosis. Concurrent with the chemotherapy and radiation therapy this patient received up to 40 g/day of ascorbic acid either orally or intravenously, as well as up to 12 g of niacin, 1000 mcg of selenium, and other vitamins and minerals. The patient stated that after his cancer had been treated for one year and he was in remission, he took himself off all the supplements. After 2-3 months the tumor recurred, so he resumed taking the vitamins (12 g ascorbic acid, 3 g niacin, and other vitamins and minerals). Since 1985 there was no further recurrence of his lymphoma despite no additional conventional anticancer therapy. He remains well. Case 324. 61-year-old woman with squamous cell carcinoma of the lung This patient was found to have a 9x10 cm mass in the lower lobe of her right lung, with CT scan evidence of subcarinal adenopathy. Mediastinoscopic biopsy of three lymph nodes were negative, but squamous cell carcinoma was diagnosed on a subsequent transthoracic needle biopsy. In October, 1990, the oncologist concluded that the cancer was Stage T2 N2 MO. He arranged for a 29-day course of radiotherapy but doubted a prolonged survival because of the large size of the primary lesion. In December, the lung mass was slightly smaller. In April, 1991, it was concluded that the lung mass was about the same size as before radiotherapy. In June, 1991, it was concluded that there might be improvement in the lung mass. In July, 1991, she began 12g vitamin C, 1.5 g niacinamide, B complex vitamins, vitamin E 1200 IU/day and other vitamins and minerals, remaining on this program thereafter. In April, 1996, a chest x-ray and CT scan examination was reported as showing no sign of tumor. In 1998 she was well. Case 384. 46-year-old woman with ovarian cancer This woman was found to have a Stage IIIB papillary serous cystoadenocarcinoma of the ovary on exploratory laparotomy for a painful abdominal mass. She was deemed to fall into the high risk treatment category and was given 6 cycles of cisplatin chemo-therapy completed in July, 1991. She achieved a sustained complete clinical remission but, because of the complication of peripheral neuropathy, was started on ascorbic acid 12 g, niacinamide 1.5 g/day, B complex, folic acid, and other vitamins and minerals. She remains in clinical remission. Conclusion I treated the first few patients with orthomolecular therapy because there was no other treatment available, because I was curious what the vitamin regimen might do and because I knew that my patients could not be harmed by giving them vitamins. As my experience with the use of multivitamins increased I became more confident that there was some value in this treatment by increasing longevity and improving the quality of life, but I did not conclude that I had fully established the validity of the program. I hoped that one day this volume of data might arouse the interest of research physicians in the field who could then conduct definitive experiments which would answer the questions: (1) Is the addition of megavitamin therapy, especially vitamin C, of value in the treatment of cancer? (2) What is the relative value of each of the nutrients and is the value of some so small that it need not be included? (3) What additional nutrients, antioxidants, etc. would improve these therapeutic results? (4) We cannot stop the search, for the results of treatment are simply not good enough with or without megavitamin therapy. We cannot stop our search until each case of cancer can be treated as easily as most infections are today and, even more importantly, until we have isolated those factors which are responsible for the major increase in the incidence and prevalence of cancer. References
termination of the study and a comparison of survival times of cancer patients receiving large regular oral doses of vitamin C and other nutrients with similar patients not receiving those doses. J Orthomol Med, 5: 143-154, 1990. Reprinted in, Cancer and Vitamin C, Cameron E, Pauling L, Camino Books, Inc. P.O. Box 59026, Phil. PA, 19102, 1993.
| |||||||||

This website is managed by Riordan Clinic
A Non-profit 501(c)(3) Medical, Research and Educational Organization
3100 North Hillside Avenue, Wichita, KS 67219 USA
Phone: 316-682-3100; Fax: 316-682-5054
© (Riordan Clinic) 2004 - 2024c
Information on Orthomolecular.org is provided for educational purposes only. It is not intended as medical advice.
Consult your orthomolecular health care professional for individual guidance on specific health problems.