 |

|
 |

|
 Back to 1999 2nd Quarter Table of Contents
Back to 1999 2nd Quarter Table of Contents
I have just finished reading A. Hoffer’s excellent new book Vitamin B3 Schizophrenia: Discovery Recovery Controversy.1 He certainly make a convincing case that the methyl acceptors, niacin and niacinamide, by reducing the availability of noradrenalin and adrenalin and hence of the toxin adrenochrome, are effective in the treatment of some schizophrenics. I cannot help feeling, however, that these relationships are only part of a larger puzzle. In the United States, schizophrenia is commonest where fodder crops are low in selenium, and hence where this trace element is deficient in the food chain.2,3 In addition, Buckman and colleagues4 discovered that, in schizophrenics, there was a strong negative correlation between the activity of the seleno-enzyme glutathione peroxidase in platelets and erythrocytes and computed tomography scan measures of brain atrophy and increased ventricle-brain ratios. Many schizophrenics, therefore, are glutathione peroxidase deficient and this seleno-enzyme lack appears associated with serious brain damage. In addition, Rudin and colleagues5 have had some success in the treatment of schizophrenia with linseed oil, but argue that supplementing the diets of schizophrenics with essential fatty acids is successful only when selenium intake is optimum. To quote these authors directly, “If a primate is deficient in the antioxidant element selenium, providing supplemental essential fatty acids will only make the selenium deficiency worse. Whatever selenium stores are in the body will be used up that much sooner in an attempt to protect the EFA [essential fatty acids] from oxidative damage”. Interestingly, as early as 1979 Vaddadi6 reported that a combination of penicillin and evening primrose oil (which contains both linoleic and gamma linoleic acid) had a dramatic positive effect on some schizophrenics. It would appear, therefore, that the challenge is to show how adrenochrome excess, and selenium and essential fatty acid deficiencies somehow combine to promote schizophrenia. In the spirit of de Bono,7 who considers that no new idea is bad, since even if wrong, it may stimulate others to find the truth, I am willing to make an initial attempt to identify such links between the adreno-chrome and prostaglandin hypotheses. Maiorino and co-workers8 have shown that the glutathione peroxidases are characterized by a catalytically active selenium which forms the center of a strictly conserved triad composed of seleno-cysteine, glutamine and tryptophan. This combination seems to optimize the reactivity of selenium, increasing its ability to protect against free radical damage. As explained in the book1 tryptophan is also a precursor of niacin and this vitamin can, in fact, be manufactured from it in the body. It seems therefore, that tryptophan is needed to produce both niacin and glutathione peroxidase. Since niacin is a methyl acceptor that slows the formation of adrenalin and hence adrenochrome, by making less noradrenalin available, it follows that a deficiency of tryptophan is likely to be linked to an excess of adreno-chrome. However, since tryptophan is a precursor of glutathine peroxidase, a deficiency of this amino acid is likely also to cause an inadequacy of this seleno-enzyme. Obviously, in addition, glutathine peroxidase deficiencies might be due to depressed selenium intake, or to a lack of seleno-cystein and/or glutamine.8 Peng and Yang,9 in a study of Kaschin-Beck Disease, which is endemic in selenium deficient regions of China, discovered that selenium and adrenalin were antagonistic. To quote them directly “A model test of adrenalin auto-oxidation was carried out, [on human embryonic cartilage cells] and it was found that the oxyradical can be eliminated by Se(IV). Thus, it was assumed, that selenium was a protective factor and free radical scavenger for Kaschin-Beck Disease.” This evidence seems to suggest that, like niacin, both selenium and its associated enzyme glutathine peroxidase reduce human adrenalin and hence adrenochrome levels. In addition, Baez and co-workers,10 have shown that adrenochrome is efficiently conjugated with glutathione in the presence of human glutathione transferase, providing protection against neurodegenerative diseases. There is also some evidence that glutathione disulfide may interfere with the formation of adreno-chrome by scavenging free radicals.11 If glutathine peroxidase is protective against adrenochrome, Rudin and colleagues’5 observation that giving schizophrenics essential fatty acids, without extra selenium, worsens their symptoms can be explained. This would occur, as the authors point out, because already depressed glutathione peroxidase stores would be depleted further by attempting to protect essential fatty acids from oxidative damage. This in turn would mean that any selenium-related reduction in adrenalin and hence in adrenochrome would cease, adrenochrome levels would rise and schizophrenic symptoms would worsen. Similarly, since schizophrenics produce abnormally high levels of adrenochrome, it is not surprising that they are typically glutathione peroxidase deficient.4 This is because if this seleno-enzyme is required to detoxify adrenochrome, as suggested here, then its stores are likely to be depressed in schizophrenics by a constant demand for this purpose. This lack of glutathione peroxidase in schizophrenics, in turn, would cause excessive oxidation of the essential fatty acids and would hence lead to the failure of the formation and action of prostaglandins.12 It is possible that such essential fatty acid and associated postaglandin deficiencies could account for the brain atrophy and increased ventricle-brain ratios identified in schizophrenics by Buckman and co-workers.4 There may be yet another available piece to the puzzle. The metabolism of selenium involves its methylation.13 Berry14 has suggested that the methyl acceptor niacin reduces such selenium methylation and prolongs its action in the body. That is, niacin and selenium may themselves be synergistic and may act more effectively together. Interestingly, Shultz and Leklem15 have shown that blood selenium levels are significantly and positively correlated with those of niacin, suggesting this may indeed be the case. In conclusion, if the ideas put forward here are correct, then the Hoffer1 adreno-chrome and the Horrobin12 prostaglandin hypotheses are not in conflict. Rather, they are the beginning and end of a chain of events that lead to schizophrenia. If so, the orthomolecular treatment of schizophrenia should involve at least two steps. Initially, niacin and selenium should be added to diet, in an attempt to lower adrenochrome levels while simultaneously increasing those of glutathione peroxidase. Perhaps trytophan, cysteine and glutamine might also be required. It should be noted, however, that there is some evidence that cysteine may increase the damaging effects of adrenochrome.16 Once both adreno-chrome and glutathione peroxidase levels have normalized, essential fatty acids, including those present in evening primrose oil, would be added to the protocol. The goal here would be to help normalize prostaglandin activity in the brain. I hope readers of JOM find this letter provocative. Please feel free to look for holes in the hypotheses it presents. Harold D. Foster, Ph.D. University of Victoria P.O. Box 3050, Victoria, BC V8W 3P5 References
Journal of Orthomolecular Medicine Vol. 14, No. 2, 1999
Euthyroidism Cannot be Restored by Thyroxine Alone The goal of replacement therapy in hormone deficiencies is to restore a physiologically natural state so that all the patient’s symptoms due to hormone deficiency are alleviated. Despite the fact that replacing thyroid hormone with thyroxine (T4) alone has long been known to not result in a physiologically natural state, it is advocated and often done for hypothyroid patients. It is advocated by some that patients not receive preparations containing triiodothyronine (T3). Bunevicius et al. have shown that their hypothyroid patients had more symptoms alleviated by replacement therapy with thyroxine plus triiodothyronine than by thyroxine alone.1 Figure 1 (p. 113) shows the normal range for T4, T3 and the relationship between T4 and T3 in euthyroid subjects2 (hexagon), the normal relation between T4 and T3 in hypothyroid subjects3 on T4 therapy alone (shaded region) and the average values of T4 and T3 for Bunevicius et al. patients on T4 alone (circle), or T4 + T3 (square). Bunevicius et al. show that therapy which provides a more physiologically natural relationship between T4 and T3 is more effective at alleviating hypothyroid symptoms. This would appear to resolve the debate over treatment of hypothyroidism in favor of those using combinations of T4 and T3 rather than T4 alone. The typical “4:1” combination products containing bothT4 andT3 provide about twice as high a ratio of T3 to T4 as Bunevicius et al. used, which would be expected to place their total T4 and T3 values in the middle of the physiologically normal range as shown by the cross. Andrew Hall Cutler, Ph.D. 10 Thunder Run #28c Irvine, CA 92614-7034 References 1. Bunevicius R, Kazanavicius G, Zalinkevicius R, Prange A: Effects of thyroxine as compared with thyroxine plus triiodothyronine in patients with hypothyroidism. N Engl J Med, 1999; 340: 424-9.
Figure 1. Normal range for T3 and T4 and the relationship between T3 and T4 in euthyroid subjects. 3 4 5 6 7 8 9 10 11 12 13 14 15 Total T4, μg/dl 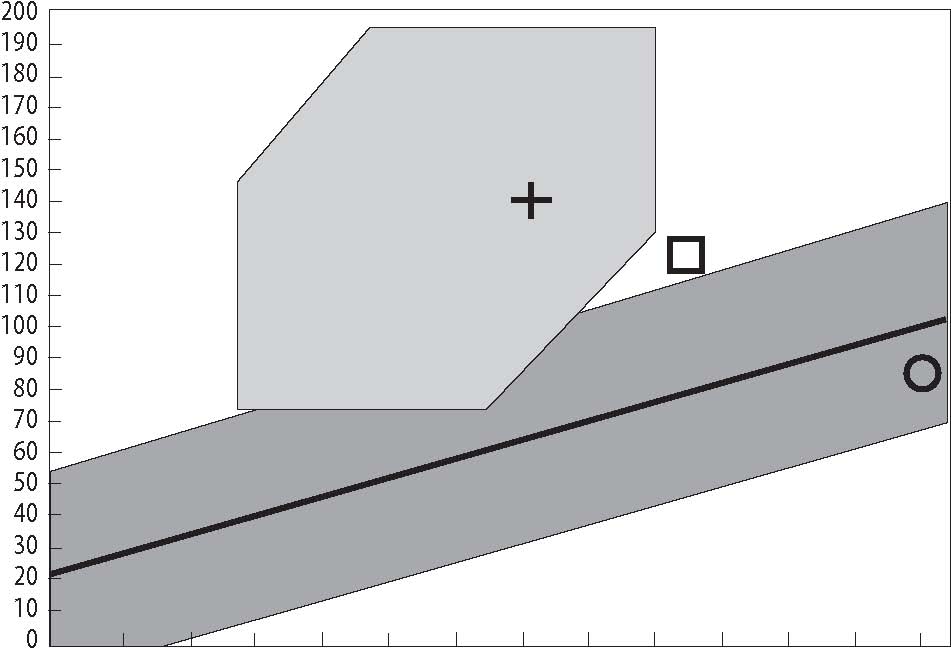 A Personal Experience of Schizophrenia the psychiatric establishment. Impoved by Vitamin Therapy In about 1979 I was involved in the To Dr. Hoffer: delivery of community mental health serv- This is a fan letter to Dr. Hoffer which ices in a small Canadian community. A ought to have been sent more than 30 years young woman came to see me. I knew her ago. as a Junior High School teacher with an From 1964 to 1968 I was a student excellent reputation as both a teacher and nurse. During my student years passing an involved member of our community. reference was made in the classroom to the She was newly married and I believe ex-work Hoffer was doing in Saskatchewan in pecting her first child at the time. She the area of vitamin therapy for the treat-lived an ordinary but productive life. What ment of schizophrenia. Many of the senior was extraordinary about her was that she nurses on the wards were quite excited had been diagnosed with schizophrenia and about his work and the possibilities it had after enduring the terrible effects of the for normalizing the lives of those with pharmaceutical and other treatments of schizophrenia in our care and particularly schizophrenia common then, and unfortu-those who were newly diagnosed. Later, we nately still common now, her parents sought heard that he had left Saskatchewan and out Dr. Hoffer who placed her on what was that his valuable work was being deni-called megavitamin therapy in those days grated or at least not taken seriously by and her condition stabilized. The hallucinations and behaviours associated with schizophrenia vanished and she was living the life of a healthy young woman. Her visit to me was for the purpose of letting me know that she was being treated by Dr. Hoffer. She told me that if she ran into any difficulties she did not want to turn to the medical establishment for assistance because she was concerned that she would be medicated and subjected to the treatments that had been imposed upon her in the past. She said that if she encountered any difficulties she would come to see me with the understanding that I would provide her with assistance knowing that her wish was to remain on the orthomolecular program. Some years later she came to see me again. By then she had a second child. Her concern was that she felt her mental stability was threatened, she felt unwell and was hearing voices. I suggested she telephone Dr. Hoffer at once. She had a conversation or two with him over the telephone and adjusted the vitamins she was taking, based on his advice.Within the next few months she flew to British Columbia to see him. During the ensuing years until I left that community she remained well. I often saw her and we would exchange small knowing smiles. She shared the nature of her diagnosis with very few people because the social stigma of being diagnosed with schizophrenia could well have jeopardized her place in both the education system and the society in which we lived. She was one of Dr. Hoffer’s many successes and she is one of those people upon whom a strong community fabric is built. It saddened me no end to read a newspaper article in January, 1999, which stated that Hoffer’s psychiatric colleagues still lumber along in their dinosaur world believing that a chemical straightjacket which removes all traces of personality is a suitable treatment. Wrong! In my work as a lawyer these many years later, I still deal with families whose lives have been torn apart by family members with schizophrenia who prefer no treatment at all or even death over the drugs available to them. Not uncommonly, I am approached by grandparents whose biological schizophrenic children have produced offspring they cannot care for because of their disease. The grandparents often have to engage in bitter legal battles with their own beloved children in order to salvage the lives of their grandchildren. All too often I represent a spouse in legally dissolving a marriage dismembered by the decades of emotional upheavals the couple suffer as a result of parenting children with schizophrenia who have conducted their lives in the often painful and irrational ways. As so it goes. Dr. Hoffer’s far ahead of his time and while most schizophrenics have not benefited from his work because of the resistance of the medical community, there are many individuals and their families whose lives would be very different without him. He deserves great honour and respect. May I add my voice to the chorus of gratitude. Thank you. (Name witheld by request) Orthomolecular Help Following Stroke I am writing this letter to express appreciation to the field of orthomolecular medicine and its intrepid practitioners. They have made life in our family infinitely easier for which we will be forever grateful. I would like to share one example. In 1974 my husband suffered a severe stroke. Thinking he needed the best medical care, I asked his GP to call in a specialist (my first major mistake). The GP engaged a brain surgeon. I know now that if you bring in a surgeon you can expect surgery. The surgeon wanted to do exploratory surgery reasoning that he could not tell whether the blob on the X-Ray was a blood clot or a tumor. In hindsight I question whether it was necessary and perhaps the ten hour operation did more damage than the stroke since the problem area was deeply embedded near the brain stem. He was given a slim chance of survival but 11 weeks later he surprised everyone and returned home from the hospital. He had always been covered with a sheet in the hospital so I was shocked when I saw his condition. At 6 feet tall with a normal weight of 172 lbs. he then weighed 122 lbs. Although not paralyzed, the damage was in the cerebellum which governs muscle control giving him slurred speech, a severe balance problem, and jerky movements. These weren’t his only problems. He had been a loving husband and father, always good humored, generous and kind. Now he had became suicidally depressed, pathologically jealous, and sometimes verbally and physically violent with a very low frustration level. Thinking that his symptoms were all a result of the stroke, for six or seven years I tried to find help from orthodox medicine. We went to local MDs, to mental health and University health clinics (second mistake). They were always happy to accept the insurance money to do batteries of testing but always the same conclusion was that they had nothing to suggest other than a tranquilizer. In 1980 I ran across one of Dr. Hoffer’s books which described his work with schizophrenia and depression. I also read of his study with Canadian POWs who had been starved in Japanese camps for 44 months. All became very ill physically, and some mentally ill. A few who took vitamin B3 became normal. They needed megadoses–at least 3 grams daily. They were also given vitamin C. Dr. Hoffer’s surprising success with intractable mental disorders started me to wonder whether my husband’s mental condition was more a result of his nutritional state due to deprivation in the hospital and not from the stroke damage. Having no experienced health professional to turn to who could oversee “the experiment,” I decided that there was little to lose and put my husband on a regimen of about 1500 mg of B3 (combination of niacin and niacinamide), plus “bowel tolerance” doses of vitamin C and the complete B complex of 50 to 100 mg of each, plus minerals and a few other supplements. I expected no miracles from a man who for seven years had sat all day, head down, twiddling his thumbs and saying, “give me a gun and I’ll get out of your life.” In about three weeks I was shocked to hear him In the other room laugh out loud at a TV program. This was from a person who had not even smiled sincerely for seven years. Slowly the paranoia and jealously left. He became much calmer, began cracking jokes, cooperating and was entering the real world. Instead of constant criticism he even began to sympathize with the family’s disruption. I kept him on this regimen for several years. In the early months, if I forgot or gave him less than 1500 mg of B3, the depression would return. Slowly, I tapered off the large doses and his mental state remained relatively even. In June of 1989 some months after a bad fall which crushed some vertebrae, he contracted chronic lymphatic leukemia. Literature suggests that leukemia sometimes follows a broken bone. Hal Huggins, DDS, has discovered a connection with this particular kind of leukemia and mercury poisoning (My husband had had a tooth filIed with silver amalgam just prior to the fall. The dentist forgot my standing order that no teeth in our family were to be filled with mercury). In October of 1991 he died of heart failure due, possibly, from the additional mercury in conjunction with a dose of chemotherapy he chose to take over my strong objections. Thanks to Linus Pauling and the orthomolecular approach, my husband was never hospitalized nor did he suffer any side effects with the chemotherapy. During his struggle with leukemia he never came down with an infection which couldn’t be handled by immediately using herculean doses of vitamin C at the first sign of a problem (people don’t die of leukemia, the doctor told us, they die of an infection). At the time of death his WBC count was 150,000 but he died at 80 ... quietly and painlessly in his sleep. Janet Pettit 164 Heatherly Heights Road Saluda, North Carolina 28773 |

This website is managed by Riordan Clinic
A Non-profit 501(c)(3) Medical, Research and Educational Organization
3100 North Hillside Avenue, Wichita, KS 67219 USA
Phone: 316-682-3100; Fax: 316-682-5054
© (Riordan Clinic) 2004 - 2024c
Information on Orthomolecular.org is provided for educational purposes only. It is not intended as medical advice.
Consult your orthomolecular health care professional for individual guidance on specific health problems.